Wolff-Parkinson-White syndrome (WPW)
Cudurka 'Wolff-Parkinson-White (WPW)' waa xaalad ay ku jirto waddo dheeraad ah oo koronto oo wadnaha ah taasoo u horseedda xilliyo garaaca wadnaha oo degdeg ah (tachycardia).
Cudurka 'WPW syndrome' waa mid ka mid ah sababaha ugu badan ee dhibaatooyinka garaaca wadnaha degdegga ah ee dhallaanka iyo carruurta.
Caadi ahaan, calaamadaha korantada waxay raacaan waddo gaar ah oo loo maro wadnaha. Tani waxay caawineysaa wadnaha inuu si joogto ah u garaaco. Tani waxay ka hortageysaa wadnaha inuu yeesho garaac ama garaac dheeraad ah oo dhakhso u dhaca.
Dadka qaba cudurka WPW syndrome, qaar ka mid ah calaamadaha korantada ee wadnaha waxay maraan waddo dheeri ah. Tani waxay sababi kartaa garaaca wadnaha oo deg deg ah oo loo yaqaan 'supraventricular tachycardia'.
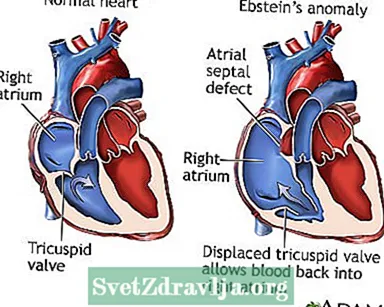
Inta badan dadka qaba cudurka WPW syndrome ma laha wax dhibaato kale oo wadnaha ah. Si kastaba ha noqotee, xaaladdan waxaa lala xiriiriyay xaalado kale oo wadnaha ah, sida Ebstein anomaly. Nooca xaalada ayaa sidoo kale ku dhaca qoysaska.
Intee jeer ayuu garaaca wadnaha degdega ahi dhacaa way ku kala duwan yihiin hadba qofka. Dadka qaarkood ee qaba cudurka WPW syndrome waxay leeyihiin dhowr jeer dhacdooyin xaddiga garaaca wadnaha oo deg deg ah. Qaar kale waxay yeelan karaan garaaca wadnaha degdega ah hal mar ama laba jeer usbuucii ama in ka badan. Sidoo kale, waxaa laga yaabaa inaysan jirin wax calaamado ah haba yaraatee, sidaa darteed xaaladdaas waxaa la helaa marka baaritaanka wadnaha la sameeyo sabab kale.
Qofka qaba cilladan waxaa laga yaabaa inuu qabo:
- Laab xanuun ama laab xanuun
- Dawakhaad
- Madax-fudeyd
- Suuxdin
- Jasbado (dareen ah inaad dareento garaaca wadnahaaga, badanaa si dhakhso ah ama aan caadi ahayn)
- Neefta oo kugu yaraata
Baadhitaan jireed oo la sameeyo inta lagu jiro dhacdada tachycardia ayaa muujin doonta garaaca wadnaha oo ka dhakhso badan 100 garaac daqiiqadii. Qiyaasta garaaca wadnaha ee caadiga ah waa 60 ilaa 100 garaac daqiiqaddii dadka waaweyn, iyo in ka yar 150 garaac daqiiqad kasta dhallaanka, dhallaanka, iyo carruurta yaryar. Cadaadiska dhiiggu wuxuu ahaan doonaa mid caadi ah ama hooseeya kiisaska badankood.
Haddii qofku uusan qabin tachycardia waqtiga baaritaanka, natiijooyinka waxay noqon karaan kuwo caadi ah. Xaaladda waxaa lagu ogaan karaa ECG ama kormeerka ambalaaska ECG, sida kormeeraha Holter.

Tijaabad loo yaqaan 'electrophysiologic study (EPS)' waxaa lagu sameeyaa iyadoo la isticmaalayo tuubbooyin qalbiga lagu dhejiyo. Tijaabadani waxay kaa caawin kartaa aqoonsiga meesha marinka korantada ee dheeriga ah.
Daawooyinka, gaar ahaan daawooyinka antiarrhythmic drugs sida procainamide ama amiodarone, ayaa loo isticmaali karaa in lagu xakameeyo ama looga hortago garaaca wadnaha oo deg deg ah.
Haddii xaddiga garaaca wadnuhu uusan caadi ku soo laaban daaweyn caafimaad, dhakhaatiirtu waxay isticmaali karaan nooc daaweyn ah oo loo yaqaan 'cardioversion koronto' (shoogga).
Daaweynta muddada-dheer ee cudurka WPW syndrome badanaa waa kala-soocid kateetarka. Nidaamkani wuxuu ku lug leeyahay gelinta tuubo (kateetarka) xididka xidid yar oo u dhow gumaarka ilaa aagga wadnaha. Marka caaraddu gaadho wadnaha, aagga yar ee keenaya garaaca wadnaha degdegga ah ayaa la baabi'iyaa iyadoo la isticmaalayo nooc gaar ah oo tamar ah oo loo yaqaan 'radiofrequency' ama la qaboojiyo (cryoablation). Tan waxaa loo sameeyaa iyada oo qayb ka ah daraasadda elektrophysiologic (EPS).
Qalitaanka wadnaha ee furan si loo gubo ama loo xayiro marinka dheeriga ah waxay sidoo kale daaweyn joogto ah u noqon kartaa cudurka WPW. Xaaladaha badankood, nidaamkan waxaa la sameeyaa oo keliya haddii aad u baahan tahay qalliinka wadnaha sababo kale awgood.
Kala soocida kateetarka ayaa daaweysa cilladaan dadka badankood. Heerka guusha ee hawshu wuxuu u dhexeeyaa 85% ilaa 95%. Heerarka guusha way kala duwanaan doonaan iyadoo kuxiran goobta iyo tirada wadiiqooyinka dheeraadka ah.
Dhibaatooyinka waxaa ka mid noqon kara:
- Dhibaatooyinka qalliinka
- Wadne istaag
- Cadaadiska dhiigga oo yaraaday (waxaa sababa garaaca wadnaha oo deg deg ah)
- Dhibaatooyinka ay keento daawooyinka
Qaabka ugu daran ee garaaca wadnaha degdega ah waa wadnaha wadnaha (VF), oo si dhakhso leh ugu horseedi kara shoog ama dhimasho. Waxay mararka qaarkood ku dhici kartaa dadka qaba WPW, gaar ahaan haddii ay sidoo kale qabaan wadna garaac aan caadi ahayn (AF), taas oo ah nooc kale oo ka mid ah garaaca wadnaha aan caadiga ahayn. Noocan garaaca wadnaha degdegga ahi wuxuu u baahan yahay daaweyn degdeg ah iyo nidaam loo yaqaan 'cardioversion'.
Wac daryeel caafimaad bixiyaha haddii:
- Waxaad leedahay astaamo cudurka WPW.
- Waxaad qabtaa cilladan iyo astaamuhu way ka sii darayaan ama kuma fiicnaanayaan daaweynta.
Kala hadal daryeel bixiyahaaga haddii xubnaha qoyskaaga laga baarayo qaababka la iska dhaxlay ee xaaladan.
Cilladda uur qaadista; WPW; Tachycardia - Wolff-Parkinson-White syndrome; Arrhythmia - WPW; Wadna garaac aan caadi ahayn - WPW; Wadna garaac dhakhso leh - WPW
 Cillad-xumada Ebstein
Cillad-xumada Ebstein Holter kormeerka wadnaha
Holter kormeerka wadnaha Nidaamka wadista wadnaha
Nidaamka wadista wadnaha
Dalal AS, Van Hare GF. Khalkhal gelinta heerka iyo laxanka wadnaha. Gudaha: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Buugga Buugga Caafimaadka Caruurta. 21aad ed. Philadelphia, PA: Elsevier; 2020: baab 462.
Tomaselli GF, Zipes DP. U dhowaanshaha bukaanka qaba wadnaha wadnaha. Gudaha: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Cudurka Wadnaha ee Braunwald: Buugga Buugta Daawada Wadnaha iyo Xididdada. 11aad. Philadelphia, PA: Elsevier; 2019: cutubka 32.
Zimetbaum P. Wadna xanuunka wadnaha ee 'Supraventricular arrhythmias'. Gudaha: Goldman L, Schafer AI, eds. Daawada Goldman-Cecil. 26aad. Philadelphia, PA: Elsevier; 2020: baab 58.
